For most patients with endometrial cancer (EC), surgery is the go-to option to make sure as much of the cancer is removed as possible. When the surgery involves the removal of the ovaries (oophorectomy), your body will be forced into menopause unless you’ve already gone through it naturally. This process is called surgical menopause..
Knowing what to expect during surgical menopause can help you feel better prepared for what’s to come following your oophorectomy.
Do all patients with endometrial cancer need an oophorectomy?
Not all patients with EC need to have their ovaries removed. Sometimes, younger patients with early-stage, non-aggressive forms of EC are given the option to remove their uterus but keep their ovaries, which prevents surgical menopause from occurring. However, this may increase the likelihood of the cancer coming back.
Read more about EC treatment and care
For others, surgery isn’t an option for a number of reasons, in which case chemotherapy or radiation may be used instead.
If you are given the choice, make sure to take the time to weigh the risks and benefits of receiving an oophorectomy before deciding what’s right for you and your health. Your doctor can also walk you through the details and give you advice that is tailored to your medical history.
What does surgical menopause feel like?
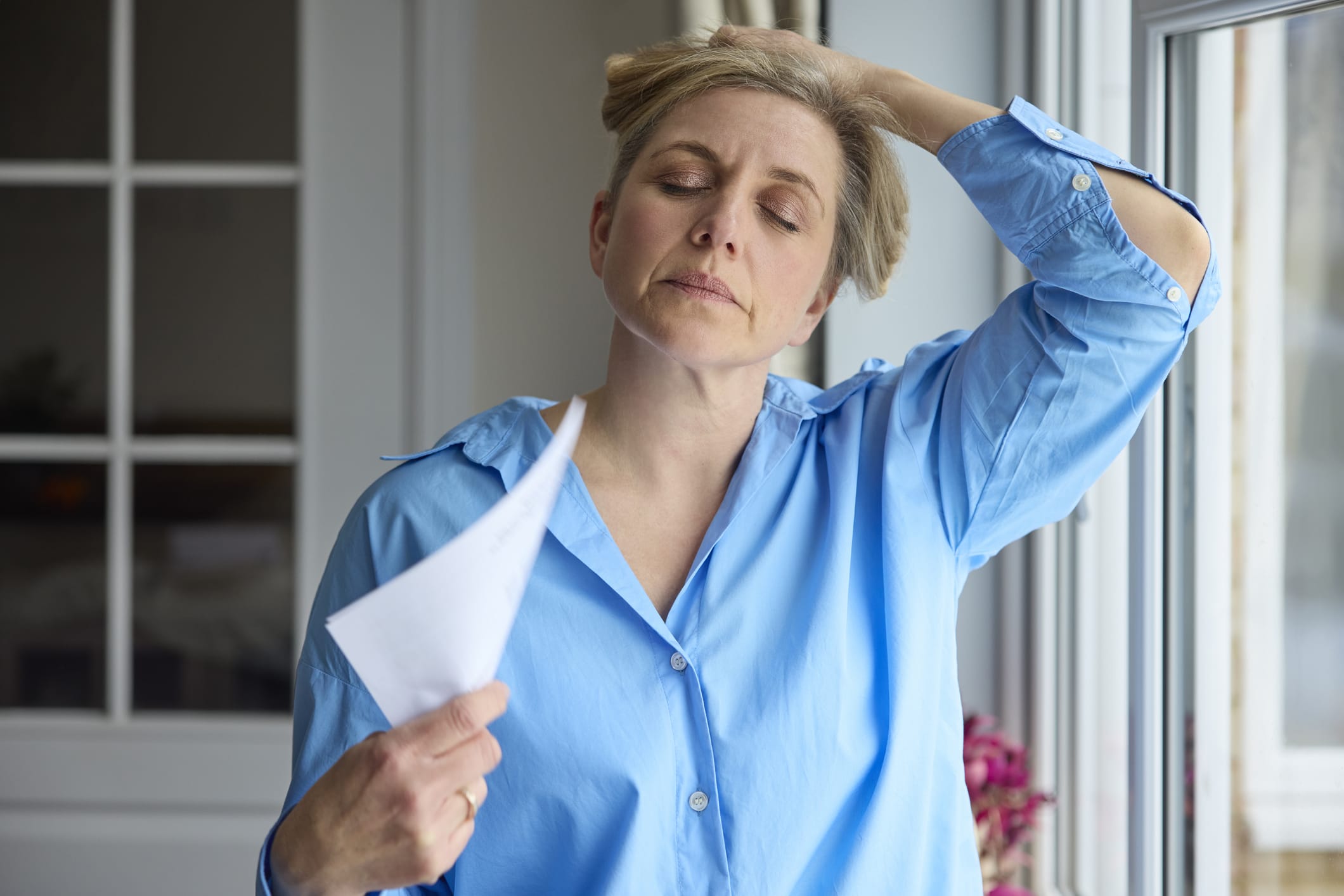
Once both of your ovaries are removed, the body will immediately go into surgical menopause. In general, the symptoms are the same as those of natural menopause, including:
- Hot flashes
- Night sweats
- Vaginal dryness
- Hair loss
- Trouble sleeping
- Mood swings and irritability
The main difference between surgical and natural menopause is that you may feel the symptoms of surgical menopause more strongly due to the sudden drop in estrogen levels, as opposed to the more gradual decline that happens during natural menopause.
Menopause can also increase your risk of osteoarthritis or heart disease down the line. More research is needed on how the long-term effects of surgical and natural menopause differ, though.
How is surgical menopause managed?
For some, dietary modifications can provide relief from the symptoms of menopause. Make sure to eat plenty of fruits and vegetables, and try to avoid caffeine if you’re having trouble sleeping, especially later in the day.
If you don’t already, consider incorporating exercise into your daily routine. This can be something as simple as some light stretching or dancing to keep your body moving. If you feel up to it, pilates or lifting weights will also help to keep your bones and muscles strong.
Most healthcare professionals recommend a calcium intake of up to 1,200 mg and a vitamin D intake of about 600 international units (IU) to lower the risk of osteoporosis. You can reach these numbers through a combination of diet and supplements (but talk to your doctor before adding any new supplements to your routine).
There is still very limited evidence as to whether hormone replacement therapy poses any risks to those who have had EC. Because EC is “fed” by estrogen, there is some fear that giving patients estrogen could cause any remaining cancer cells in the body to grow. Overall, though, the current data appears to support the use of estrogen therapy in patients with EC who are experiencing surgical menopause.
Sign up here to get the latest news, perspectives, and information about EC sent directly to your inbox. Registration is free and only takes a minute.