CANCÚN, Mexico—Women in the United States are now more likely to die of endometrial cancer (EC) than of ovarian cancer, according to new research presented at the International Society of Ultrasound in Obstetrics and Gynecology’s ISUOG 2025 conference here.

And women of color are especially at risk, said Ohad D. Rotenberg, MD, an obstetrician-gynecologist at Montefiore Einstein in New York City.
“Many countries have adopted colorblind data collection policies to avoid racial bias. But this has led to unintended consequences,” he said, warning that ultrasound alone may not be reliable for detecting EC in Black women.
One reason, he said, is their increased likelihood of uterine fibroids, making it difficult to visualize the endometrium. The other is women of color are far more likely to have type 2 endometrial cancer—the kind that is not caused by obesity.
“It’s not estrogen‑induced, and there is a consensus that because it’s coming out from a lining which is thin, ultrasound will not detect it. You need a biopsy to make a definitive diagnosis.”
He added: “Ovarian cancer definitely has always been considered much more lethal. You’d rather have endometrial cancer than ovarian cancer, God forbid. But as a population, mortality rates in EC—unlike most other cancers—are increasing mainly because of increased obesity.”
Dr. Rotenberg was among several experts to speak about EC at this year’s Sept. 14-17 ISUOG gathering, which took place for the first time in Mexico.
The link between EC and obesity
Elisabeth Epstein, MD, is a Swedish cancer specialist with the Department of Clinical Science and Education at Stockholm South Hospital. She was very blunt as to why EC rates are going up.
“Endometrial cancer is one of the most common gynecological malignancies. It’s rising because it’s correlated to adiposity (the accumulation of body fat), and there are more obese people now,” said Dr. Epstein, who also works at Sweden’s Karolinska Institute.
She added, “90% of women who get EC present with abnormal bleeding, most commonly after menopause. It’s really important to see your doctor if you have any bleeding abnormalities or bleeding at all after menopause.”
The best way to prevent endometrial cancer is to not be obese in the first place, Dr. Epstein advised. In addition, she said, “you shouldn’t take continuous oral hormone therapy without any progesterone if you have your uterus in place.”
Yet 10% of women with EC will not have any bleeding at all, she cautioned.
“This can be especially prevalent if you’ve had any surgery [on] your cervix,” said the Swedish physician, who has been working with diagnostic imaging for decades and has run large, multicenter studies on women with endometrial cancer. “For example, in any prolapse surgery, they remove the cervix and then stitch it together. Blood might stay in the cavity and not come out.”
The average age of women Dr. Epstein has treated is 65, though the youngest was 29.
“EC can also affect young women. If it’s a really early cancer, we can offer a fertility‑sparing treatment, but this is only for young women with hereditary endometrial cancer and no children,” she said, adding that generally, EC is treated only by removal of the uterus.
Contraception can dramatically reduce a woman’s chances of getting endometrial cancer.

A 2021 study of about 250,000 British women showed that those who took birth control pills were 20% less likely to develop breast cancer, 42% less likely to get ovarian cancer and 57% less likely to get EC. For all three cancers, the longer they took the pills, the greater the reduction.
Estrogen levels, which may be higher in patients with obesity, have the opposite effect. Prominent New York City gynecologist Steven Goldstein—who specializes in treating abnormal vaginal bleeding, ovarian masses and fibroids—said obesity is a major factor in what he calls “garden variety type 1” endometrial cancer.
“Estrogen is the culprit, and obese women will make a non-ovarian cancer form aromatization of androgens [convert androgens, such as testosterone, into estrogens] in adipose tissue, which is why obese women have more EC but less osteoporosis,” he explained. “If you see an EC in a younger woman, they’re often obese as well—and like most malignancies, the incidence of this cancer increases with age.”
The importance of EC symptom awareness
In 2009, the American College of Obstetricians and Gynecologists proposed that women with post-menopausal bleeding (PMB) and an endometrial echo less than or equal to 4 mm did not need an endometrial biopsy.
“Recently, there has been tremendous publicity in some circles that this may not be reliable in African-American women, and because they have so many more fibroids. They also have a slightly increased risk of type 2 cancers, which are known as papillary serous tumors as opposed to adenocarcinomas,” Dr. Goldstein explained. “They usually arise in a backdrop of atrophy rather than a backdrop of hyperplasia. They don’t usually have the risk factors of obesity and increased estrogen production.”
Unfortunately, the value of transvaginal ultrasound is diminished by these fibroids, he said.
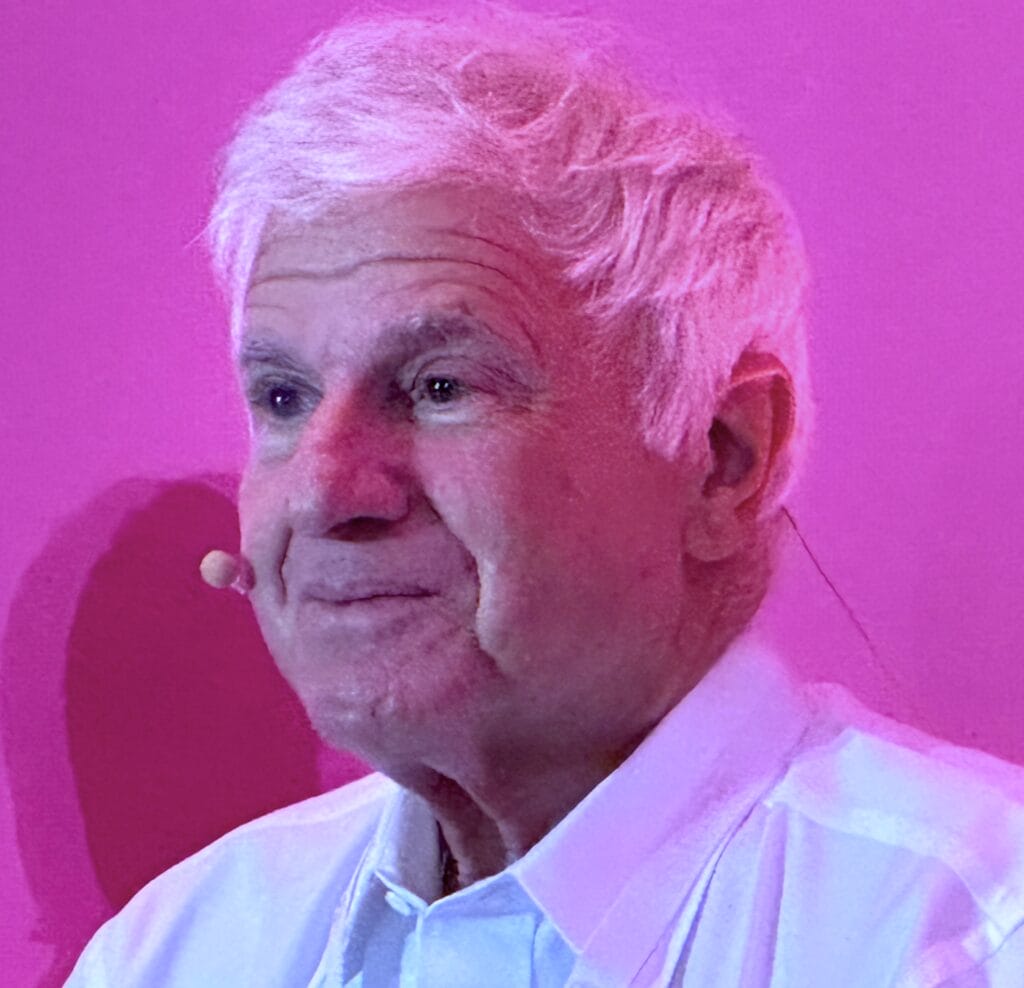
“If you cannot see the endometrial echo in its entirety, then you can’t use ultrasound. You must see the echo in its entirety,” Dr. Goldstein explained. “When we don’t see the echo sufficiently, we often will put fluid or gel in. That’s called a saline infusion, of histogram in order to see better. Dr. Rotenberg’s paper basically showed that once you have completion ultrasound, the detection or the reliability of ultrasound in Black women was every bit as good as white women.”
A big problem, said Dr. Goldstein, is an overwhelming ignorance of endometrial cancer among all women, regardless of race. He cited a 2024 survey conducted among random attendees at the Minnesota State Fair. He said 37% of the women polled weren’t aware that PMB, staining or spotting might be a sign of uterine cancer. In addition, more than 40% of these women said that if they had one episode of bleeding, they wouldn’t even call their doctor.
Even more surprisingly, 53% of respondents said their doctor had never asked if they had bleeding after menopause or discussed how important it is to be aware of it.
“What is true is that African-American women with fibroids have had so much irregular or heavy bleeding in their 30s and 40s, that when they have an episode of PMB, they may be less likely to report it because it’s like, ‘I’ve seen this movie before.’ What we really want is to decrease mortality from this disease,” Dr. Goldstein said. “If women are treated within the first eight weeks of their bleeding, their prognosis is every bit as good as if you had somehow fortuitously found it before they bled.”
In fact, more than 90% of women treated in the early stage of EC are cured. “But a number of women don’t report it or get delayed in diagnosis either because of denial, access of care, or not understanding what it is. That’s one of the reasons why mortality is on the rise.
Obesity and smoking are obvious risk factors for EC, he said, along with lack of exercise.
“That goes along with maintaining a healthy body weight, but I’m not sure exercise per se is going to prevent individual cancers. In general, women who exercise a lot are less likely to be obese than people who are not.”
“We should be spreading the message that any bleeding, staining or spotting in post‑menopausal women needs to be taken seriously and reported immediately—not wait for a second bleed, not poo-poo it and not assume this is their period returning.”
